Obesity has become a global epidemic affecting hundreds of millions of people. In the United States alone, roughly 42% of adults had obesity as of 2020, and worldwide the number of people living with obesity is expected to reach 1 billion by 2030. Carrying excessive body fat isn’t just a cosmetic concern – it is a serious health issue linked to increased risks of diabetes, heart disease, and other illnesses. Tackling obesity safely and effectively is a major challenge. Clinical trials play a vital role in developing new treatments, from breakthrough medications to innovative procedures. These studies allow researchers to test promising therapies under careful oversight, helping find better ways to achieve weight loss and improve health.
Looking for safe and effective weight loss options?
Obesity is a serious health condition, but new treatments are being developed every day through clinical trials. By joining a trial, you gain access to expert medical supervision, innovative therapies, and close health monitoring. Take the first step toward exploring options that could make a lasting difference.
Types of Obesity
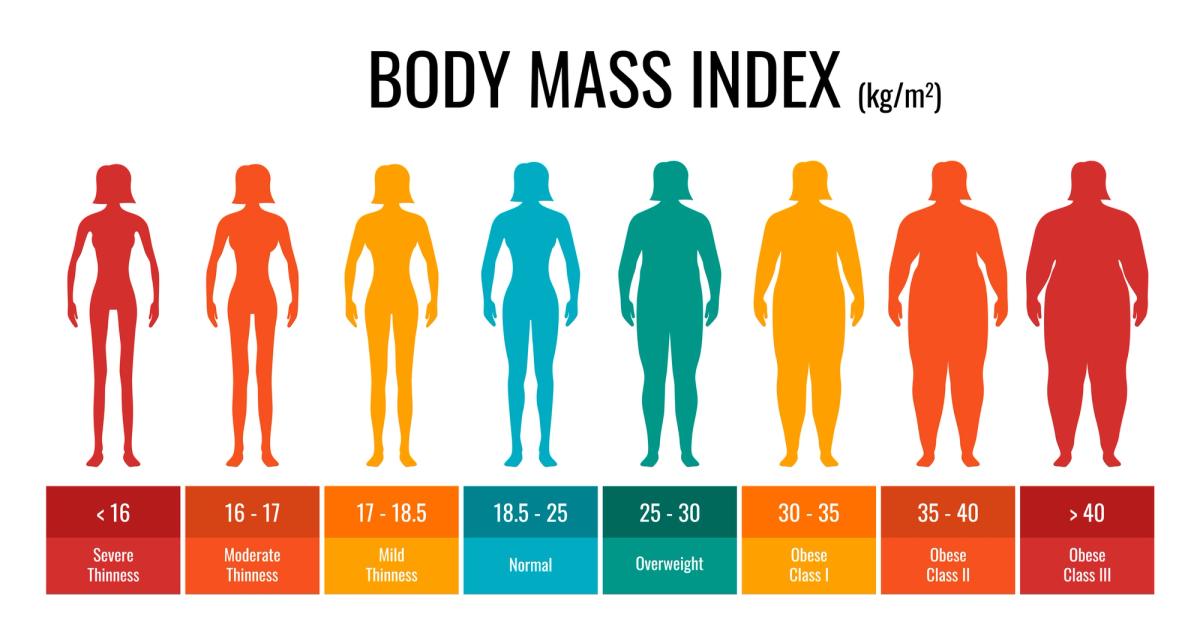
Obesity is not a single condition but rather a spectrum that varies in severity and in how fat is stored in the body. Doctors often use Body Mass Index (BMI) to classify obesity, which is calculated by comparing a person’s weight to their height. A BMI of 30 or higher is considered obese. Within this category, there are three levels. Class 1 obesity refers to a BMI between 30 and 34.9. Class 2 obesity includes a BMI from 35 to 39.9. Class 3 obesity is defined as a BMI of 40 or higher and is also called severe or extreme obesity. This last category carries the highest health risks, and the likelihood of developing life-threatening conditions such as heart disease or diabetes increases with each step up in class.
But BMI alone does not tell the full story. Where fat is stored in the body can be just as important as how much there is. Subcutaneous fat is found just under the skin and is the soft, pinchable fat in places like the hips, thighs, and arms. While too much of it can still cause strain, it is generally less dangerous than visceral fat. Visceral fat sits deeper inside the abdomen, surrounding vital organs like the liver and intestines. This type of fat cannot be pinched and is often associated with a firm, apple-shaped belly. Visceral fat is particularly harmful because it disrupts hormones, fuels inflammation, and contributes to high cholesterol, insulin resistance, and high blood pressure.
Because visceral fat carries such serious health risks, doctors often measure waist size or waist-to-hip ratio in addition to BMI. Even at the same BMI, someone with more belly fat may face higher risks than someone whose weight is concentrated in the lower body. Understanding the difference between subcutaneous and visceral fat helps guide treatment decisions. For example, losing visceral fat, even without dramatic changes in total weight, can significantly improve health outcomes. Recognizing both the severity of obesity and the type of fat involved allows healthcare providers to create more tailored and effective treatment plans.
Obesity and Morbidity
Morbidity refers to illness or disease, and obesity significantly increases the risk of developing many chronic health problems. Carrying excess fat affects nearly every organ system, from the heart and blood vessels to the liver, kidneys, lungs, joints, and even the brain.
Cardiovascular disease is one of the most serious consequences of obesity
Extra body fat raises blood pressure, increases cholesterol, and promotes clogged arteries. Over time, these changes lead to a much higher risk of heart attacks, congestive heart failure, and stroke.
Type 2 diabetes is strongly linked to obesity
When the body becomes less responsive to insulin, blood sugar levels rise. Nearly 90 percent of adults with type 2 diabetes are overweight or obese. The good news is that weight loss often improves blood sugar control and can even send diabetes into remission.
Metabolic syndrome and fatty liver disease are also common in people with obesity
Metabolic syndrome is a cluster of conditions—high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat, that together sharply increase the risk of diabetes and heart disease. Obesity is also the leading cause of non-alcoholic fatty liver disease, in which fat builds up in the liver and can progress to inflammation or scarring.
Certain cancers occur more often in people with obesity, including breast, colorectal, uterine, kidney, and liver cancers
Researchers believe that excess fat releases hormones and growth factors that encourage tumor growth. Estimates suggest that about 40 percent of cancers in the United States are diagnosed in people who are overweight or obese.
Respiratory issues are another common consequence
Extra fat around the chest and abdomen restricts lung expansion, making breathing more difficult. Obesity also greatly increases the risk of obstructive sleep apnea, where breathing repeatedly stops during sleep. Many people find that losing weight improves both sleep apnea and asthma symptoms.
The strain of extra weight also affects the joints and spine
Obesity is a leading cause of osteoarthritis, especially in the knees and hips, and contributes to chronic back pain. Even a small amount of excess weight puts disproportionate pressure on the joints, leading to pain, stiffness, and mobility problems over time.
Obesity can also impact mental health
People with obesity are more likely to experience depression, anxiety, and low self-esteem. The relationship often works in both directions—mental health struggles can make weight control harder, while obesity itself can worsen emotional well-being. Weight-related stigma and discrimination add to this burden.
Perhaps most concerning is that obesity often leads to multiple health problems at once. It is common for a person with obesity to have high blood pressure, diabetes, and arthritis together. Studies show that individuals with obesity are several times more likely to suffer from multiple chronic conditions than those at a healthy weight. The likelihood of having two or three illnesses at the same time rises sharply as BMI increases. This is why obesity is recognized as a chronic disease that requires long-term management and care.
Obesity and Mortality
Beyond causing illness, obesity can also shorten life expectancy. Researchers often describe this in terms of mortality risk, which refers to the risk of death from any cause. Studies have consistently shown that higher levels of obesity are linked to a greater chance of dying prematurely, especially from heart disease and other cardiovascular conditions. For example, people with a BMI of 35 or higher (Class 2 or Class 3 obesity) have been found to face nearly triple the risk of dying from any cause compared to people with milder obesity. Severe obesity (Class 3, or BMI 40 and above) is associated with an even greater increase in mortality, with some studies showing a five- to sixfold higher risk of death compared to people at a healthy weight.
The effect on life expectancy is striking. Large studies have shown that extreme obesity can shorten lifespan by more than a decade. In the most severe cases, individuals may lose between 6 and 14 years of life compared to peers at a normal weight. To put this into perspective, the effect of extreme obesity on life expectancy can be as harmful as, or even worse than, the effects of lifelong heavy smoking. Even moderate obesity can take years off one’s life; for example, having a BMI between 30 and 35 is linked to a reduction of about three years on average.
The main drivers of this increased mortality are the chronic illnesses closely tied to obesity. Heart attacks, strokes, diabetes complications, certain cancers, and liver disease are among the leading causes of early death in people with obesity. Excess fat places extra strain on the heart, promotes artery damage, and can trigger life-threatening events like heart failure or sudden cardiac arrest.
Fortunately, losing weight can reverse much of this risk. Research shows that even a modest weight loss of 5 to 10 percent of body weight can significantly lower blood pressure, improve blood sugar and cholesterol levels, and reduce the chances of heart attacks and strokes. Larger weight losses of 15 to 20 percent or more can lead to even greater health benefits. In this sense, weight loss is not only about appearance or comfort but about survival. Each percentage of weight reduced can translate into better odds of living a longer and healthier life.
The Importance of Safe Weight Loss
Many people with obesity want to lose weight, but how weight loss is achieved matters just as much as the result. Rapid or extreme methods often do more harm than good. Fad diets, crash diets, or “quick fix” supplements may promise fast results, but they usually lead to nutritional deficiencies, muscle loss, or health complications. Harsh workout routines can cause injuries or exhaustion, and most of these approaches are impossible to maintain long term.
Because obesity is a chronic condition, short-term fixes don’t work. Experts recommend slow, steady weight loss of about one to two pounds per week. Although this may seem modest, it is safer, more sustainable, and more likely to lead to lasting success. Losing weight too quickly often means losing water and muscle rather than fat, and the weight usually comes back.
Safe weight loss is best done under medical supervision. Doctors or dietitians can help design a plan that takes existing health conditions into account, ensures proper nutrition, and recommends the right level of physical activity. This is especially important for people who also have high blood pressure, diabetes, or other conditions that need to be carefully managed.
How Is Obesity Treated?
Treating obesity usually requires a comprehensive approach. There is no single cure, but combining lifestyle changes, medications, and sometimes surgery can help people lose weight and keep it off. The best treatment depends on the severity of obesity, overall health, and personal preferences.
Lifestyle Changes: Healthy Eating and Exercise
The foundation of obesity treatment is improving diet and physical activity. A healthy eating plan focuses on whole foods such as vegetables, fruits, lean proteins, whole grains, and healthy fats while cutting back on sugary drinks, processed snacks, and high-calorie fast foods. Small, sustainable changes—like swapping soda for water or choosing fruit instead of candy—help reduce calories without extreme restriction.
Exercise is equally important. Activities like brisk walking, swimming, dancing, or cycling help burn calories, build muscle, and improve overall health. Experts recommend at least 150 minutes of moderate activity per week, but even small increases in daily movement can make a difference. Consistency matters more than intensity, and the best exercise is the one you can enjoy long term.
Medications and Weight-Loss Drugs
When lifestyle changes alone are not enough, prescription medications can provide extra support. These drugs are usually recommended for people with a BMI of 30 or higher, or 27 with an obesity-related condition like diabetes or high blood pressure.
Some medications suppress appetite, making it easier to eat less. Others block fat absorption. The most effective new options are GLP-1 receptor agonists, such as semaglutide and tirzepatide, which mimic natural hormones to reduce hunger and slow digestion. These medications can help people lose 15–20 percent of their body weight, but they are most effective when paired with healthy habits. Since weight often returns after stopping them, they are usually prescribed as long-term therapies.
Bariatric Surgery
For people with severe obesity, especially those with a BMI of 40 or higher, or 35 with serious health conditions, bariatric surgery may be recommended. Procedures such as gastric bypass or sleeve gastrectomy shrink the stomach and change how food is processed, leading to significant and lasting weight loss.
On average, patients lose 20–35 percent of their starting weight and often see major improvements in conditions like diabetes, sleep apnea, and high blood pressure. Surgery also reduces long-term mortality, but it comes with risks and requires lifelong changes in diet, exercise, and vitamin supplementation.
Interested in how bariatric surgery impacts blood sugar and diabetes? Research is ongoing to better understand the full benefits of these procedures beyond weight loss. This clinical study is specifically examining the effects of bariatric surgeries on glucose metabolism and related health outcomes.
Learn More About the Bariatric Surgery StudyLatest Advances in Obesity Treatment
Game-Changing Medications
The biggest leap has come from a new class of drugs called GLP-1 receptor agonists. Medications like semaglutide (Wegovy®) and tirzepatide (Mounjaro®) mimic natural gut hormones that control appetite and digestion. On average, people lose 15–20 percent of their body weight with these treatments—results once only seen with surgery. Even newer drugs, like retatrutide, are showing even greater promise in early studies, with some participants losing nearly a quarter of their body weight.
Combination Therapies
Scientists are testing whether combining drugs can boost results. For example, adding anti-inflammatory agents to GLP-1 medications may help patients lose more weight while also protecting muscle mass. These “cocktail” approaches could become the future of obesity treatment, much like combination therapies already used for conditions such as high blood pressure.
Endoscopic Procedures
Less invasive than surgery, endoscopic procedures are performed through the mouth with no external cuts. One example, the endoscopic sleeve gastroplasty, uses an internal suturing device to shrink the stomach. Patients often lose 15-20 percent of their weight with quicker recovery times. New trials are testing enhancements, like combining stomach reshaping with treatments that reduce hunger hormones, potentially making these procedures nearly as effective as surgery without the same risks.
Brain and Neurological Research
Obesity is also closely tied to brain activity. Researchers are studying how the brain processes hunger, cravings, and stress. Tools like brain imaging and non-invasive stimulation are being explored to “reset” hunger signals and reduce overeating. Devices that target the vagus nerve, which helps control appetite, are also under investigation. While early-stage, this research could open new doors to treating obesity at its neurological roots.
Other Emerging Approaches
Scientists are exploring the gut microbiome, gene therapies for rare obesity syndromes, and dual-hormone medications that combine GLP-1 with other signals to enhance weight loss. Some research is even looking at ways to convert energy-storing white fat into energy-burning brown fat.
The Role of Clinical Trials in Obesity Care
For people seeking new ways to manage obesity, clinical trials can be an option. These are carefully designed research studies that test new medications, procedures, or behavioral programs under the supervision of doctors and researchers. Trials follow strict safety standards, and participants are monitored closely throughout the process.
Joining a clinical trial can provide access to investigational treatments that are not yet available to the public. Many studies cover the costs of the treatment being tested, as well as medical check-ups and support during the study. Participants often appreciate the opportunity not only to try new approaches but also to contribute to research that may benefit millions of others in the future.
Finding the right trial usually starts with searching by condition and location. Many studies are designed for adults with a BMI of 30 or higher, and some focus on specific health concerns such as diabetes, high blood pressure, or sleep apnea. Trial listings typically include the purpose of the study, what type of treatment is being tested, the length of the study, and basic eligibility criteria like age or BMI range. From there, people can answer a few screening questions online or contact the research team to learn more.
Participation is always voluntary. The process usually begins with a phone call or online screening, followed by an in-person visit where the research team explains the study in detail. Volunteers can ask questions, review consent forms, and decide whether to take part. Even after enrollment, participants can withdraw at any time if they no longer wish to continue.
Clinical trials can be a valuable way to receive attentive care, nutritional and lifestyle guidance, and potentially access new therapies before they become widely available. For people living with obesity, they represent both a personal opportunity and a chance to contribute to medical progress in this rapidly advancing field.
What to Expect in an Obesity Clinical Trial
If you join a clinical trial for obesity, the experience usually follows a structured process. While each study is different, most include the following steps:
Screening and Enrollment
The process starts with a screening visit to see if you qualify. You’ll review and sign an informed consent form, which explains the study and any risks. Doctors will check your medical history, record measurements like height and weight, and run basic tests such as blood work or vital signs.
Curious about how eligibility is determined in clinical trials? Learn more in our detailed guide that explains the key criteria researchers use to decide who can safely participate.
Baseline Measurements
Before starting treatment, researchers collect initial data. This might include surveys about diet and lifestyle, blood tests, or scans to measure body fat. These measurements give a starting point for comparison once treatment begins.
Treatment Phase
This is the main part of the study. Depending on the trial, you might receive a medication (real drug or placebo), undergo a procedure, or participate in a behavioral program. Regular study visits are scheduled to track your weight, health, and any side effects. Some trials last a few months, while others may continue for a year or more.
Follow-Up and Monitoring
After treatment ends, many studies include a follow-up period to see if results last. Researchers may schedule check-ins to track weight changes and health outcomes. Throughout the trial, safety is a priority, and you can contact the study team at any time with questions or concerns.
Completion
At the end of the trial, you may have an exit visit with final tests or surveys. Some studies offer “open-label extensions,” where participants can keep receiving the treatment after the main study ends, if it shows promising results.
Participating in a trial does require time and commitment, such as attending clinic visits and filling out food or symptom diaries. However, many people find it rewarding. You receive close medical supervision, learn more about your health, and may gain access to treatments not yet available to the public—all while contributing to research that could help others in the future.
Summary
Obesity is a complex disease that affects nearly every aspect of health, but treatment options have never been stronger. From lifestyle changes and medical support to powerful new medications and minimally invasive procedures, safe and sustainable weight loss is more achievable today than ever before.
Clinical trials play a central role in these advances. Every effective therapy we have was once tested by volunteers, and ongoing studies continue to shape the future of obesity care. By joining a trial, participants gain access to promising new treatments under expert supervision while contributing to discoveries that help millions.
Most importantly, obesity is not a personal failure—it is a medical condition that deserves compassion and evidence-based care. With science-driven treatments, supportive healthcare teams, and continued research, the path toward healthier weight and longer life is clearer than ever.
FAQs
What is the best treatment for obesity?
There isn’t one treatment that works for everyone. The best approach depends on your weight, health conditions, and personal needs. For some, lifestyle changes like healthy eating and regular activity are enough. Others may benefit from medications that reduce appetite or help control cravings. For people with severe obesity, bariatric surgery can provide the most dramatic results. The “best” treatment is usually a personalized combination that is safe, effective, and sustainable long term.
Are clinical trials for weight loss safe?
Clinical trials are designed with participant safety as the top priority. Before starting, you’ll go through a detailed screening process to make sure it’s safe for you. During the trial, doctors monitor your health closely with regular visits and lab tests. While all medical studies carry some risk, most side effects reported in obesity trials are mild and manageable. You also have the right to leave a trial at any time if you’re uncomfortable.
What are the new GLP-1 drugs?
GLP-1 drugs are a new class of medications that mimic hormones in the gut to reduce hunger, control blood sugar, and slow digestion. The most well-known are semaglutide (Wegovy®) and tirzepatide (Mounjaro®). In studies, people taking these drugs lost 15-20% of their body weight on average - levels once thought possible only with surgery. They’re given as weekly injections and are changing how doctors treat obesity.
Are there non-surgical options for weight loss?
Yes, and most people start here. Non-surgical options include lifestyle programs (diet and exercise), prescription medications, counseling or behavioral therapy, and newer minimally invasive procedures like endoscopic sleeve gastroplasty. These approaches can lead to meaningful weight loss, especially when combined. Surgery is usually reserved for people with severe obesity or those who haven’t succeeded with other methods.
What happens during a clinical study?
You begin with a screening to check eligibility, then sign an informed consent form. Once enrolled, you may receive either the treatment being tested or a placebo. You’ll attend regular visits where the team tracks your weight, health, and any side effects. Safety is monitored closely, and at the end, you may have follow-up visits or be invited to continue in an extension study. Many participants value the close medical attention and the chance to try new therapies under supervision.
How long does it take to lose weight with new treatments?
It depends on the method. Lifestyle changes alone may lead to slow but steady weight loss (1–2 pounds per week). Medications like GLP-1 drugs usually produce noticeable results in the first few months, with continued loss over a year. Surgery or endoscopic procedures often result in faster weight drops within the first 6-12 months.
Will I regain weight after treatment?
Weight regain is possible if the treatment is stopped, especially with medications. That’s why many therapies are designed for long-term use or maintenance. Combining treatments with healthy lifestyle habits gives the best chance of keeping weight off.
How much time does a clinical trial take?
It varies. Some last just a few months, while others may run for a year or more. You’ll usually need to attend regular clinic visits (sometimes weekly, sometimes monthly) and complete surveys or check-ins. The study team will explain the time commitment before you enroll.
Will I be paid to join a clinical trial?
Many trials compensate participants for their time, travel, or expenses. The amount varies by study. Even if payment is modest, participants often find value in the medical care, monitoring, and access to new treatments.
Wondering how much participants actually get paid? Compensation in clinical trials can vary a lot depending on the study’s length, requirements, and location.
