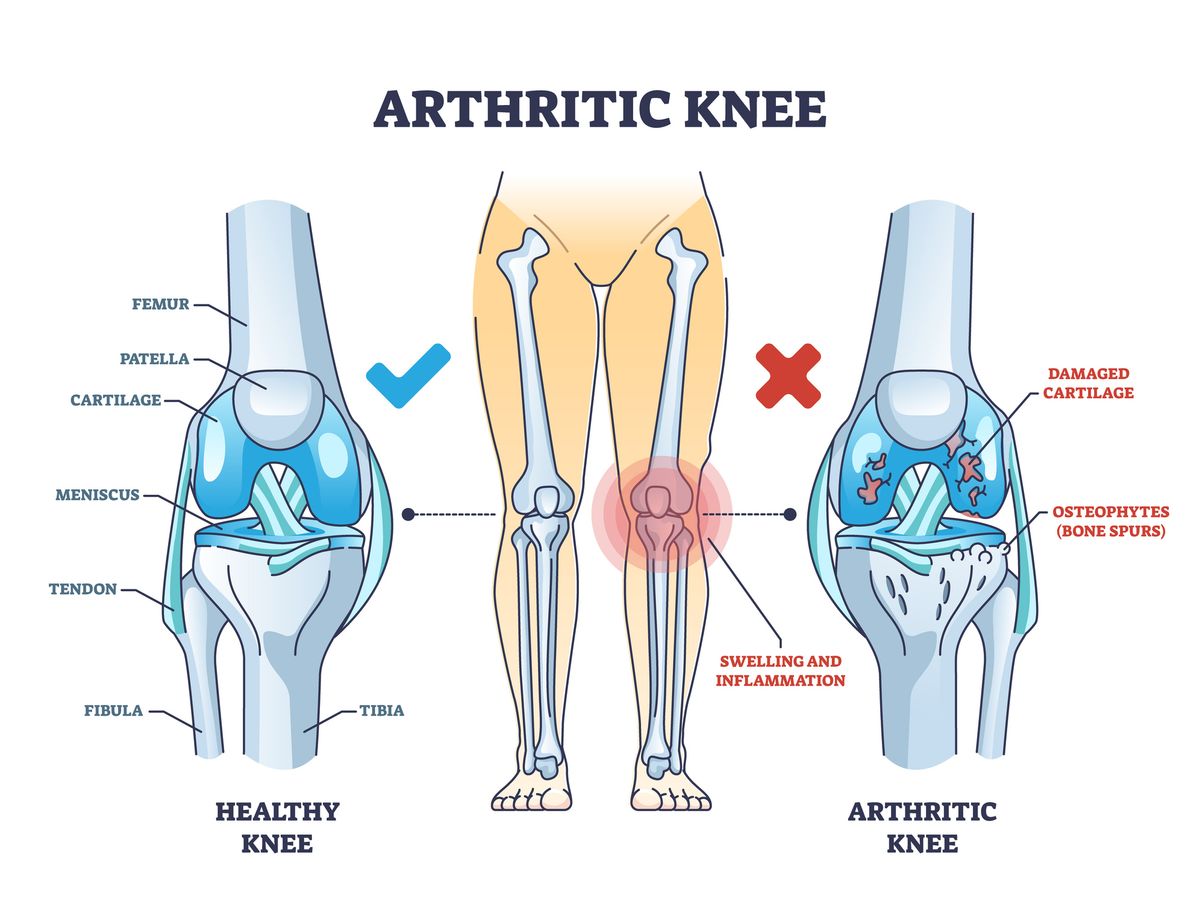
Living with osteoarthritis (OA) can be challenging, but understanding your condition and knowing about available treatments can empower you to manage symptoms and maintain a good quality of life. Osteoarthritis is the most common form of arthritis, affecting millions worldwide (about 32.5 million adults in the U.S. alone). Often called a “wear and tear” arthritis, it occurs as the protective cartilage that cushions the ends of bones in your joints gradually breaks down. Without this smooth cartilage, bones begin to rub against each other, leading to joint pain, stiffness, and swelling.
Interested in exploring new treatment options?
Find osteoarthritis clinical trials near you and see if you qualify.
What is Osteoarthritis?
Osteoarthritis is essentially a degenerative joint disease – think of it as the result of years of wear and tear on a joint. In a healthy joint, cartilage (a firm, rubbery tissue) covers the ends of the bones and acts like a shock absorber and lubricant, allowing smooth, pain-free movement. In osteoarthritis, this cartilage breaks down and wears away over time, causing the joint space to narrow and bones to grind against each other. The joints most often affected are those that bear weight or get heavy use: knees, hips, spine, and hands are common sites of OA damage.
Common symptoms of osteoarthritis include:
- Joint pain – an aching or sharp pain in the joint, often worse with movement or at the end of the day.
- Stiffness – especially after waking up in the morning or after a period of inactivity, usually lasting less than 30 minutes.
- Swelling and tenderness – the joint may appear slightly swollen and feel tender to touch due to inflammation.
- Reduced range of motion – you might find it harder to move the joint freely (for example, difficulty bending or straightening a knee).
- Grinding or cracking noises (crepitus) – you might hear or feel a crackling sensation in the joint when moving, caused by rough bone surfaces rubbing together.
It’s important to note that, unlike some other types of arthritis (such as rheumatoid arthritis), osteoarthritis is not a whole-body autoimmune disease – it primarily affects the joints and does not typically cause symptoms in other organs. OA can range from mild to severe. Some people experience only occasional aches, while others have chronic pain that can significantly interfere with daily activities. Age and wear are major contributors (most people over 60 have some degree of OA), but other factors like old injuries, overuse (repetitive stress), genetics, and excess body weight can increase the risk of developing osteoarthritis.
Standard Treatments (and Their Limits)
Medications
Medications are often the first line of defense for osteoarthritis pain. Over-the-counter options such as acetaminophen (Tylenol) can ease discomfort, while nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen target both pain and inflammation. These medicines provide short-term relief but do not slow the disease. Long-term NSAID use can lead to side effects such as stomach irritation, high blood pressure, or kidney problems. Stronger prescriptions or topical creams may help in tougher cases, but opioids are generally avoided because their risks outweigh the benefits for osteoarthritis.
Corticosteroid Injections
Corticosteroid injections can bring rapid relief for painful joints, especially in the knees and hips. By calming inflammation inside the joint, they can ease pain for a few weeks to a couple of months. The drawback is that the effects wear off, and repeated injections can actually damage cartilage over time. For this reason, steroid shots are usually reserved for flare-ups and not considered a long-term strategy.
Physical Therapy and Exercise
Physical therapy and exercise are essential for keeping joints as healthy and functional as possible. Strengthening the muscles around a joint provides better support, while stretching and low-impact activities like walking, cycling, swimming, or tai chi help maintain mobility and balance. Exercise also supports weight control, which can ease joint stress. The challenge is that pain may make it hard to stay active, and overexertion can cause flare-ups. A physical therapist can design a safe, personalized program to help patients stay active without aggravating symptoms.
Weight Management
Weight management plays a major role in controlling osteoarthritis symptoms. Every pound lost relieves about four pounds of pressure on the knees with every step. Even a modest loss of 5 to 10 pounds can significantly reduce pain and improve movement. While losing weight is not easy, combining healthier food choices with regular activity can be one of the most powerful self-care strategies for people with osteoarthritis.
Assistive Devices and Lifestyle Adjustments
Assistive devices and simple adjustments can make day-to-day life easier. Braces and supports can stabilize unstable joints, orthotic shoe inserts improve alignment, and canes or walkers reduce strain when walking. At home, tools like jar openers, ergonomic keyboards, and long-handled reachers can help protect joints from unnecessary stress. Learning joint-protection strategies—such as lifting with larger muscles or breaking tasks into smaller steps—can also minimize pain during daily activities.
Surgery
Surgery is generally reserved for severe cases of osteoarthritis where other treatments no longer work. The most common option is joint replacement, especially for hips and knees. During this procedure, damaged joint surfaces are replaced with artificial parts that often last 20 years or more. Surgery can dramatically reduce pain and improve mobility, but it carries risks such as infection and blood clots, and recovery requires rehabilitation. For this reason, joint replacement is considered a last resort when quality of life is significantly affected.
When Current Treatments Don’t Work
Despite the many therapies available, some people with osteoarthritis continue to struggle with daily pain and stiffness. You might be taking your medications, going to therapy, and using braces or supports—and still feel limited. Why does this happen? There are several reasons.
Osteoarthritis Is More Than “Wear and Tear”
While osteoarthritis is often described as mechanical damage to the joint, biology and the nervous system also play a role. Chronic inflammation can change how the nervous system processes pain, a phenomenon known as central sensitization. In this state, the nerves become extra sensitive and amplify pain signals. This means pain may feel worse than what the joint damage alone would suggest, and standard painkillers may not fully relieve it.
Damage Beyond What Treatments Can Fix
Most standard treatments—like medications or injections—target symptoms, not the underlying joint damage. When cartilage is almost completely worn away or bone spurs restrict movement, these therapies can only help so much. They may reduce pain temporarily but cannot restore lost cartilage or fully reverse stiffness.
Individual Differences
Every patient’s osteoarthritis is unique. Some people’s pain is driven mainly by inflammation, while others suffer more from mechanical friction between bones or from weak supporting muscles. Health conditions such as back pain, fibromyalgia, or depression can also amplify pain. Even factors like poor sleep or fatigue can lower pain tolerance and make symptoms feel worse.
Limits of Medications and Therapy
Over time, medications may lose effectiveness or side effects may prevent higher doses. For example, an NSAID might initially control pain, but stomach irritation or high blood pressure could limit its long-term use. Similarly, physical therapy and exercise can help, but progress may plateau or pain may block further improvement.
Under-Treatment or Advanced Disease
In some cases, current strategies may simply not be enough. Severe osteoarthritis may require surgery, while other patients may not have fully achieved key goals such as weight reduction or muscle strengthening. Understandably, many people hope to avoid surgery or long-term medication, but under-treating the disease can lead to ongoing pain.
New and Emerging Therapies
Exciting advances in science are opening new possibilities for osteoarthritis treatment. While these options are not yet part of routine care, many are being actively studied in clinical trials and could shape the future of how we manage this disease.
Hyaluronic Acid Injections (Viscosupplementation)
Hyaluronic acid is a natural lubricant that helps joints glide smoothly. In osteoarthritis, levels of this substance decline, making joints feel stiff and painful. Viscosupplementation involves injecting a gel-like form of hyaluronic acid into the joint, most commonly the knee, often as a short series of weekly treatments. The goal is to restore lubrication, ease stiffness, and make movement more comfortable. Some patients report several months of relief, with studies suggesting that up to two-thirds of people may benefit.
The effectiveness of hyaluronic acid injections has been debated. Some research shows only modest improvements compared with placebo, while other patients and clinicians find the results worthwhile. The therapy seems to work best for people with moderate osteoarthritis, rather than in very early or very advanced stages. Relief, when it occurs, is temporary, but injections can be repeated. Side effects are usually mild, such as temporary swelling at the injection site.
Platelet-Rich Plasma (PRP) Therapy
Platelet-rich plasma, or PRP, comes from the patient’s own blood. After a small blood draw, the sample is processed in a centrifuge to separate and concentrate the platelets, which contain natural healing factors. The concentrated plasma is then injected into the arthritic joint. The idea is that these growth factors can calm inflammation and encourage a healthier joint environment.
PRP has gained attention because of its use in sports medicine, and studies in osteoarthritis suggest it may reduce pain and stiffness for several months. Some trials even show it can outperform hyaluronic acid injections in knee osteoarthritis. Still, results vary, and because the treatment is considered experimental, it is not covered by insurance. Patients who pursue PRP usually pay out of pocket, often hundreds or even thousands of dollars. Another challenge is that PRP preparations differ from one clinic to another, which may explain why results are inconsistent. Despite these uncertainties, PRP is considered very safe because it comes from the patient’s own blood.
Stem Cell Treatments
Few experimental options generate as much public interest as stem cell therapy. The concept is appealing: using the body’s own regenerative cells to repair or even rebuild damaged cartilage. In practice, most “stem cell” treatments involve harvesting cells from bone marrow or fat tissue and injecting them into the arthritic joint.
Early research suggests these injections may reduce inflammation and improve pain and function, though true cartilage regrowth has not yet been proven. At present, no stem cell therapy is FDA-approved for osteoarthritis, and many of the procedures offered in clinics are unregulated and very costly. They can also involve invasive steps, such as bone marrow draws or liposuction. While most small studies suggest the injections are safe, experts caution that the actual number of stem cells in these preparations is very low. The benefits people report may be due more to anti-inflammatory effects than to regeneration. Clinical trials are ongoing, and for now, patients are advised to approach stem cell treatments with cautious optimism.
Biologic Drugs Targeting Inflammation
Biologic medicines—engineered antibodies or proteins—have transformed the treatment of autoimmune diseases like rheumatoid arthritis. Researchers are now exploring whether similar approaches could work for osteoarthritis by targeting the pathways that drive pain and low-grade inflammation.
One promising area of study is blocking nerve growth factor (NGF), a molecule that plays a key role in pain signaling. Trials of NGF-blocking drugs such as tanezumab have shown significant pain relief, sometimes stronger than NSAIDs, though safety concerns remain. In some patients, joint damage worsened more quickly, especially when the drugs were combined with NSAIDs. Other biologic approaches, such as targeting inflammatory proteins like IL-1 or IL-6, have so far shown limited results.
Although no biologic drug is yet approved for osteoarthritis, the research continues. Scientists are also testing advanced approaches such as gene therapy—delivering anti-inflammatory instructions directly into the joint—and experimental agents designed to preserve or even thicken cartilage. One early trial of a growth factor injection called sprifermin suggested it could increase cartilage thickness in the knee, though symptom improvement was modest.
The Future Ahead
None of these treatments are cures, and most are still focused on relieving symptoms rather than reversing the disease. But the variety of approaches being explored—from injections that improve lubrication, to regenerative techniques, to advanced biologic drugs—reflects the urgent need for better options. Clinical trials are the key step in determining which of these therapies will become safe, effective tools for people living with osteoarthritis in the years to come.
Clinical Trials for Osteoarthritis
Clinical trials are research studies where volunteers receive investigational treatments under close medical supervision. They are the foundation of medical progress—every medication, injection, or therapy we use today had to be tested in trials before becoming standard care. For osteoarthritis, there is a lot of ongoing research, ranging from new drugs to lifestyle programs.
What Happens in an OA Clinical Trial?
When you join a clinical trial, you follow a study plan (called a protocol) that explains the treatment, schedule of visits, and tests you’ll have. Osteoarthritis trials usually track outcomes like pain, stiffness, walking ability, and sometimes imaging (X-rays or MRIs) to check for structural changes in the joint.
Most studies are randomized (participants are assigned by chance to different groups), and many are placebo-controlled (some people receive a placebo or standard treatment for comparison). This design helps researchers know if the new therapy truly works. Trials are also often blinded, meaning neither you nor the researchers know whether you’re getting the experimental treatment or a placebo, to avoid bias. Throughout the study, your health is closely monitored, and safety is always the top priority.
What Kinds of Treatments Are Being Studied?
Osteoarthritis trials are exploring many different strategies. Some focus on new pain-relieving drugs or supplements that may work better than current options. Others test disease-modifying therapies—agents that aim to slow cartilage breakdown or encourage repair. Injections such as hyaluronic acid, PRP, or stem cell therapies are also being studied under more controlled conditions.
Beyond drugs, there are trials for lifestyle approaches, like specific exercise programs, weight-loss interventions, or dietary supplements (for example, collagen or turmeric). Researchers are also investigating devices and surgical techniques that might improve joint function. Essentially, any promising idea—whether it’s a pill, an injection, a procedure, or a lifestyle change—can be tested in a trial.
Who Can Join a Trial?
Each study has eligibility criteria that determine who can participate. These often include age range, type and severity of osteoarthritis (confirmed by X-ray), and past treatments. Some trials seek people who haven’t tried certain therapies yet, while others recruit those who have exhausted standard options.
Clinical trials may offer access to new therapies that could reduce pain and improve mobility.
Check your eligibility for ongoing osteoarthritis studiesSafety is also a factor. People with certain medical conditions or medications may be excluded if participation could be risky. Many trials specifically look for patients with moderate to severe osteoarthritis who are not getting enough relief from current treatments, since these are the people who need new options most.
Clinical trials are designed with your safety in mind. If you’re considering participating, start by exploring studies that match your condition and comfort level.
Benefits of Joining a Clinical Trial
- Access to new treatments: You may be among the first to try a therapy not yet available to the public.
- Extra medical attention: Trial participants often receive frequent check-ups, imaging, and lab tests, giving you more insight into your condition.
- Contribution to science: Even if the treatment doesn’t help you personally, your participation helps researchers find better options for future patients.
- Covered costs: Study medications and procedures are usually provided at no cost, and some trials reimburse travel or other expenses.
- Education and support: Many participants value the extra information and guidance they receive from research staff about living with osteoarthritis.
Risks and Considerations
Clinical trials also involve uncertainties. The treatment may or may not work, and there can be side effects not yet fully understood. You may be assigned to a placebo group, meaning you won’t receive the active treatment (though you will still get standard care). Participation also takes time—clinic visits, tests, and extra check-ins are usually required.
Before enrolling, every participant goes through an informed consent process, where all known risks and requirements are explained in plain language. You’ll always have the chance to ask questions and decide whether participation feels right for you.
Living Well With Osteoarthritis
Even though there is no cure for osteoarthritis yet, many people live active, fulfilling lives by combining medical care with healthy lifestyle choices. Managing OA is not only about medications or doctor visits—it’s also about self-care, daily habits, and mindset. Here are some proven strategies to help you feel and function better.
Eat a Joint-Healthy Diet
There’s no single “arthritis diet,” but good nutrition can make a big difference. An anti-inflammatory eating pattern, such as the Mediterranean diet, is often recommended. This means filling your plate with fruits, vegetables, whole grains, fish rich in omega-3s (like salmon), nuts, and olive oil, while cutting back on processed foods and sugars.
Certain foods may offer extra benefits—turmeric and ginger for their anti-inflammatory compounds, leafy greens for antioxidants, and fish or fish oil for omega-3s. Staying hydrated also helps keep joints moving smoothly. Supplements like glucosamine and chondroitin have mixed evidence, but some people find them helpful (always check with your doctor before trying them). Don’t forget vitamin D and calcium to keep your bones strong, especially if OA affects weight-bearing joints.
Keep Moving with Joint-Friendly Exercise
It may seem counterintuitive to exercise when your joints hurt, but movement is one of the most effective ways to manage OA. The key is low-impact activity that builds strength and flexibility without stressing the joints. Walking, cycling, swimming, water aerobics, tai chi, and yoga are all excellent choices.
Exercise strengthens the muscles that support joints, improves balance, and helps maintain mobility. It also releases endorphins—natural pain relievers that improve mood. Start gently, even with just 5–10 minutes a day, and gradually increase as you’re able. Range-of-motion stretches can prevent stiffness, while a physical therapist can design a safe plan if you’re unsure what’s right for you. Remember the phrase: “motion is lotion” for arthritic joints.
Manage Your Weight
Weight management is one of the most powerful tools for reducing OA symptoms. Every pound lost removes about four pounds of pressure from the knees with each step. Even modest weight loss—5 to 10 pounds—can significantly improve pain and mobility.
The goal isn’t appearance; it’s reducing strain on your joints and lowering inflammation. Set achievable targets, such as losing 1–2 pounds per week, and celebrate small milestones along the way. Pair a balanced diet with regular activity for the best results. If weight loss feels overwhelming, your healthcare team can connect you with nutritionists or support programs.
Protect Your Joints
Living with OA means learning to “work smarter, not harder.” Joint protection techniques reduce unnecessary strain and make daily tasks easier. Use larger muscles and joints when lifting or carrying—hold grocery bags on your forearm instead of your fingers, or lift with your legs instead of your back. Break chores into smaller steps, and take breaks often.
Assistive tools can also make a big difference: jar openers, ergonomic kitchen gadgets, raised toilet seats, or shower grab bars reduce strain. Braces, orthotics, or a properly fitted cane can improve mobility and safety. Far from being a sign of weakness, these tools preserve independence and prevent falls. Even simple changes, like placing a pillow between your knees at night, can ease hip or knee pain.
Support Your Mind and Sleep
Chronic pain doesn’t only affect the body—it can weigh heavily on mood and sleep. Stress, sadness, or anxiety can actually make pain feel worse, while poor sleep lowers pain tolerance. Building good sleep habits, like a calming bedtime routine and a supportive mattress, can break the cycle. Heat therapy before bed (such as a warm bath or heating pad) may also ease stiffness.
Relaxation techniques like deep breathing, meditation, or gentle stretching can help manage stress. Support groups, whether in person or online, connect you with others who understand the challenges of OA. If you’re feeling overwhelmed by pain or low mood, talking to a counselor or therapist can be an important step. Emotional health is just as vital as physical health in managing arthritis.
Stay Positive and Engaged
OA can change how you do things, but it doesn’t mean giving up the activities you love. With adjustments, you can keep enjoying hobbies and social life. Swap running for cycling, or use raised beds for gardening instead of kneeling. Focus on what you can do rather than what you can’t.
Setting small, realistic goals—like walking for 15 minutes a day—can build confidence and give a sense of progress. Staying engaged in meaningful activities, from playing with grandchildren to volunteering, often improves both mood and pain.
FAQs
Is osteoarthritis simply a result of aging?
While age is a risk factor, osteoarthritis is not an inevitable part of growing older. It develops through a combination of cartilage breakdown, joint inflammation, changes in the underlying bone, and even alterations in how the nervous system perceives pain. Many older adults never develop significant OA, while younger individuals can be affected if they have risk factors such as joint injury, obesity, or genetic predisposition.
Can lifestyle changes really make a difference?
Yes. Although lifestyle adjustments cannot cure osteoarthritis, they can significantly improve symptoms and quality of life. Regular low-impact exercise strengthens the muscles around joints, while weight management reduces stress on the knees and hips. A balanced, anti-inflammatory diet supports overall health and may help ease symptoms. These steps, when combined with medical treatment, form the foundation of long-term OA management.
How effective are injections for osteoarthritis?
Injections can provide meaningful relief for some patients, but the benefit depends on the type of injection and the stage of disease. Corticosteroid injections are widely used for short-term pain relief, while hyaluronic acid injections may help some individuals with moderate knee OA for several months. Newer options such as platelet-rich plasma and stem cell–based approaches are under investigation, with mixed but promising results. Importantly, no injection currently repairs lost cartilage; all aim to relieve symptoms.
When should surgery be considered?
Joint replacement surgery, particularly of the knee or hip, is usually considered when pain is severe, function is highly limited, and other therapies no longer provide relief. Modern joint replacements are highly effective for the right patient, often restoring mobility and independence for many years. However, because surgery carries risks and requires rehabilitation, it is typically reserved as a last resort when conservative treatments are insufficient.
What role do clinical trials play in osteoarthritis treatment?
Clinical trials are essential for developing new therapies. They provide patients with the opportunity to access promising treatments—such as novel biologic drugs, regenerative injections, or structured lifestyle programs—before they are widely available. Participants benefit from close medical monitoring and contribute to the scientific knowledge that shapes future care. For individuals who have not found adequate relief with standard therapies, clinical trials can be an important option to consider.
